Combined Infrared Laser and LED for Postmastectomy Pain and Discomfort: A Case Report
Mario A Trelles1 and R Glen Calderhead1,2
1: Instituto Médico Vilafortuny /Antoni De Gimbernat Foundation, Cambrils, Spain; and 2: LG Biomedical, Tochigi, and Japan Phototherapy Laboratory, Tokyo, Japan
Mastectomies can sometimes be associated with prolonged pain and discomfort. Low reactive-level laser ther-apy (LLLT) at 830 nm has been reported as effective in pain attenuation. A new generation of quasi-monochromatic light emitting diodes at a nominal 830 nm has offered the clinician an alternative IR phototherapy source for the hands-off treatment of large areas. The combination of the LED therapy over a large area combined with punctal application of laser therapy is an interesting concept. The present study eval-uated this combination phototherapy in a patient with comparatively long-term postmastectomy pain. A 44-year-old female had suffered from postmastectomy pain and discomfort for over 3 months, despite taking a nonsteroidal anti-inflammatory drug at high doses. A GaAlAs diode laser (60 mW, CW, 20 sec and 60 J/cm 2 per point) in punctal application was combined with an LED array (830 nm ± 5 nm, 20 min/irradiation, CW, 60 J/cm 2) in the dermatomal approach. Three consecutive daily sessions were given at the above parameters. The Hospital Anxiety and Depression Scale (HADS) was administered one day before and one day after the treat-ment regimen. Range of movement (ROM) and pain relief scores were recorded. The pre-and posttreatment HADS scores for depression and anxiety were 14 and 9, and 4 and 4, respectively. Pain and discomfort de-creased somewhat after the first session, and more rapidly with the subsequent 2 sessions. At 24 hours after the third session, the patient was completely pain free with a full ROM. After an 8-week follow-up, ROM was still good, but mild discomfort was noted around the right breast, and a single ‘top-up’ session with the LED array alone was required, which was effective. The combination of punctal laser and area LED therapy at 830 nm over three consecutive daily sessions improved postmastectomy pain and restored full ROM in this one pa-tient, with good latency which was extended with a single ‘top-up’ IR LED session. Further controlled studies with larger patient populations and longer follow-ups are warranted.
Comparative study using 685-nm and 830-nm lasers in the tissue repair of tenotomized tendons in the mouse
Carrinho PM, Renno AC, Koeke P, Salate AC, Parizotto NA, Vidal BC.
Laboratory of Electro-Thermo-Phototherapy, Department of Physiotherapy, Federal University of Sã o Carlos, Sã o Carlos, Brazil.
Photomed Laser Surg. 2006 Dec;24(6):754-8. [PMID: 17199477]
Objective: The objective of this study was to evaluate the effects of 685- and 830-nm laser irradiations, at different fluences on the healing process of Achilles tendon (Tendon calcaneo) of mice after tenotomy.
Background data: Some authors have shown that low-level laser therapy (LLLT) is able to accelerate the healing process of tendinuos tissue after an injury, increasing fibroblast cell proliferation and collagen synthesis. However, the mechanism by which LLLT acts on healing process is not fully understood.
Methods: Forty-eight male mice were divided into six experimental groups: group A, tenomized animals, treated with 685 nm laser, at the dosage of 3 J/cm(2); group B, tenomized animals, treated with 685-nm laser, at the dosage of 10 J/cm(2); group C, tenomized animals, treated with 830-nm laser, at dosage of 3 J/cm(2); group D, tenomized animals, treated with 830-nm laser, at the dosage of 10 J/cm(2); group E, injured control (placebo treatment); and group F, non-injured standard control. Animals were killed on day 13 post-tenotomy, and their tendons were surgically removed for a quantitative analysis using polarization microscopy, with the purpose of measuring collagen fibers organization through the birefringence (optical retardation [OR]).
Results: All treated groups showed higher values of OR when compared to injured control group. The best organization and aggregation of the collagen bundles were shown by the animals of group A (685 nm, 3 J/cm(2)), followed by the animals of group C and B, and finally, the animals of group D.
Conclusion: All wavelengths and fluences used in this study were efficient at accelerating the healing process of Achilles tendon post-tenotomy, particularly after the 685-nm laser irradiation, at 3 J/cm(2). It suggests the existence of wavelength tissue specificity and dose dependency. Further studies are required to investigate the physiological mechanisms responsible for the effects of laser on tendinuos repair.
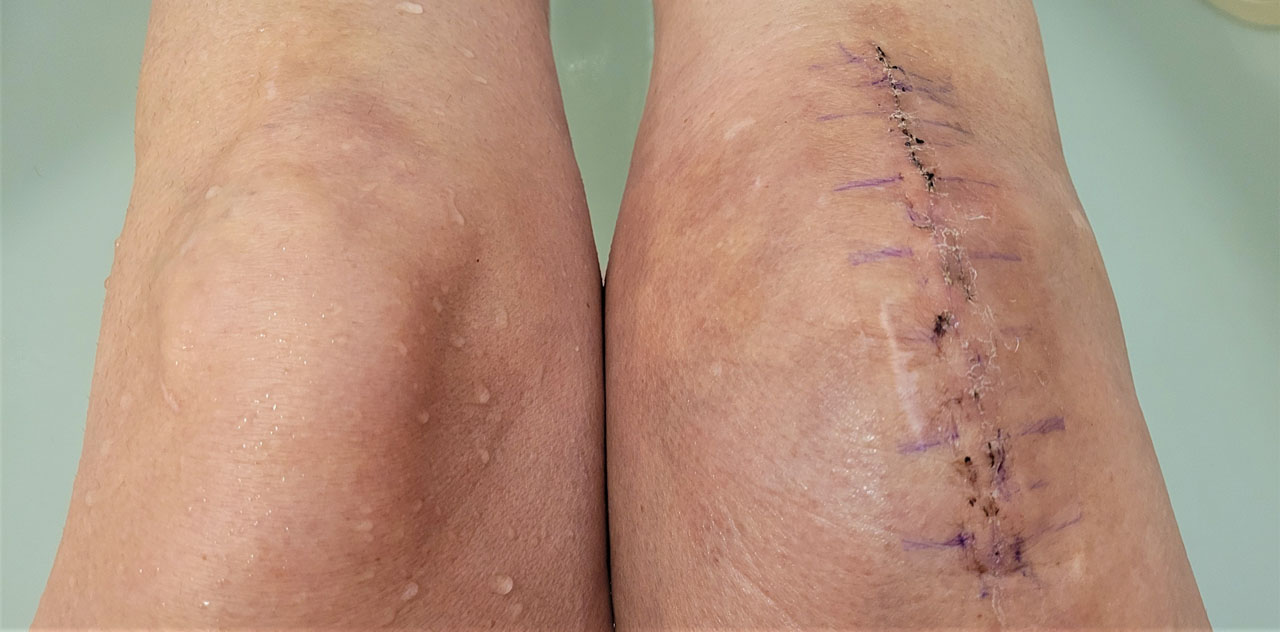
Effects of Low-Level Laser Therapy on Pain and Scar Formation after Inguinal Herniation Surgery: A Randomized Controlled Single-Blind Study
de Paiva Carvalho RL, Alcâ ntara PS, Kamamoto F, Cressoni MD, Casarotto RA.
Postgraduate Program in Rehabilitation Sciences, University of Sã o Paulo, Sã o Paulo, Brazil.
Photomed Laser Surg. 2009 Oct 12. [PMID: 19821701]
Abstract Objective: The aim of this study was to investigate the efficacy of an infrared GaAlAs laser operating with a wavelength of 830 nm in the postsurgical scarring process after inguinal-hernia surgery.
Background: Low-level laser therapy (LLLT) has been shown to be beneficial in the tissue-repair process, as previously demonstrated in tissue culture and animal experiments. However, there is lack of studies on the effects of LLLT on postsurgical scarring of incisions in humans using an infrared 830-nm GaAlAs laser.
Method: Twenty-eight patients who underwent surgery for inguinal hernias were randomly divided into an experimental group (G1) and a control group (G2). G1 received LLLT, with the first application performed 24 h after surgery and then on days 3, 5, and 7. The incisions were irradiated with an 830-nm diode laser operating with a continuous power output of 40 mW, a spot-size aperture of 0.08 cm(2) for 26 s, energy per point of 1.04 J, and an energy density of 13 J/cm(2). Ten points per scar were irradiated. Six months after surgery, both groups were reevaluated using the Vancouver Scar Scale (VSS), the Visual Analog Scale, and measurement of the scar thickness.
Results: G1 showed significantly better results in the VSS totals (2.14 +/- 1.51) compared with G2 (4.85 +/- 1.87); in the thickness measurements (0.11 cm) compared with G2 (0.19 cm), and in the malleability (0.14) compared with G2 (1.07). The pain score was also around 50% higher in G2.
Conclusion: Infra-red LLLT (830 nm) applied after inguinal-hernia surgery was effective in preventing the formation of keloids. In addition, LLLT resulted in better scar appearance and quality 6 mo postsurgery.
Laser and Sports Medicine in Plastic and Reconstructive Surgery
Junichiro Kubota M.D.
Department of Plastic and Reconstructive Surgery, Kyorin University School of Medicine, Tokyo, Japan.
Flap survival with diode laser therapy: Skin flap or graft surgery are major procedures in Plastic and Reconstructive Surgery. Skin flap necrosis has been a problem for us. The author reported on the enhanced blood flow following the low reactive laser therapy in skin flaps. The 830 nm diode laser (20 – 60 mw) irradiated flaps showed a greater perfusion, a greater number of blood vessels, and a higher rate of survival areas than the control flaps in the rat models and clinical cases. Improvement of wound healing with diode laser therapy: The diode laser therapy was indicated for traumatic skin ulcers received from sport activities and traffic accidents which had proved resistant to conservative treatment. The diode laser system has a wavelength of 830 nm. and output power of 150or 1000mw in continuous wave. The diode laser was applied with the non-contact method to the area on the wound for one minute once a day every day during the treatment period. The diode laser was used successfully for the rapid enhanced healing of traumatic skin ulcers in clinical cases.
Discussion: The majority of patients hope to avoid undergoing a surgical operation, trying instead with conservative treatments for injuries. The diode laser therapy improved the flap circulation and wound healing of severe skin ulcers. And this therapy has been applied for temporomandibular joint pain and we have obtained favorable results. The diode laser therapy has proved to be particularly effective for pain attenuation. The diode laser therapy may well offer an additional convenient, safe and side-effect free method. On the other hand, the Q-switched Nd:YAG laser system applied to the traumatic tattoos, achieving consistently good results concomitant with easy and safe operation, successfully achieving excellent lightening of the target lesions.
The Effect of Infra-Red Diode Laser Irradiation on the Duration and Severity of Post-Operative Pain: A Double-Blind Trial
Kevin C. Moore, Naru Hira, Ian J. Broome and John A. Cruikshank
Laser Therapy Volume 4: 1992 Pp: 145-148
This trial was designed to test the hypothesis that LLLT reduces the extent and duration of postoperative pain, Twenty consecutive patients for elective cholecystectomy were randomly allocated for either LLLT or as controls. The trial was double blind. Patients for LLLT received 6-8-min treatment (GaAlAs: 830 nm: 60 mWCW: CM) to the wound area immediately following skin closure prior to emergence from GA. All patients were prescribed on demand postoperative analgesia (IM or oral according to pain severity). Recordings of pain scores (0-10) and analgesic requirements were noted by an independent assessor. There was a significant difference in the number of doses of narcotic analgesic (IM) required between the two groups. Controls n = 5,5: LLLT n = 2.5, No patient in the LLLT group required IM analgesia after 24 h. Similarly the requirement for oral analgesia was reduced in the LLLT group, Controls n = 9: LLLT n = 4. Control patients assessed their overall pain as moderate to severe compared with mild to moderate in the LLLT group. The results justify further evaluation on a larger trial population.